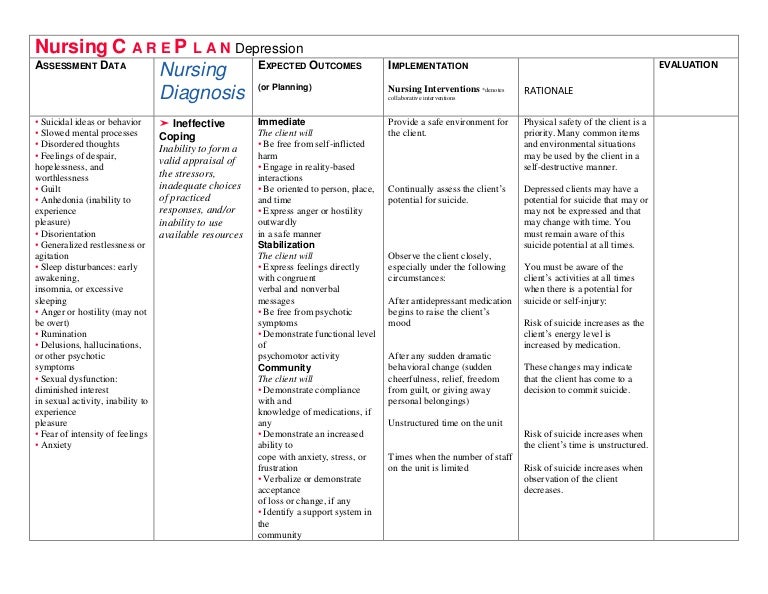
The concept of complex post-traumatic stress disorder (CPTSD) was initially proposed by Herman back in 1992 (Herman, 1992), however it has only recently been introduced as an official diagnosis within the classification manuals e.g. ICD-11 World Health Organization. It is, therefore, not that surprising that after over 3 decades of lacking a structured definition of CPTSD that there has been inconsistency in the treatment methods deployed. There are generally 2 main psychological approaches;
- a 3 phase-based protocol of stabilisation, trauma memory processing and reintegration (Cloitre et al., 2012) or;
- trauma-focused psychotherapy without stabilisation.
Stabilisation and trauma memory processing are probably relatively familiar to people and ‘reintegration’ can be considered as how to bring the new you into your day to day life (that is my simplistic interpretation of it).
Karatzias, Murphy and colleagues (2019) completed a systematic review and meta-analysis of psychological interventions for ICD-11 complex PTSD symptoms. Nevertheless, all of the studies and reviews focused on either stabilisation, or trauma memory processing, with no publications reviewed factoring in the reintegration phase. This dark corner of the knowledge woodland has also meant that there is an inconsistency with the definition of the reintegration phase and a lack of evidence about what reintegration interventions may look like.
Condon et al. chose to look at this anomaly within the CPTSD evidence base, and what better way to start than to ask a range of expert international trauma clinicians their opinions to help conceptualise the definition, composition, and key principles of delivery of reintegration.
There is a distinct lack of evidence relating to the reintegration phase of Complex PTSD treatment, i.e. how to bring the new you into your day to day life.
Methods
A range of experts were identified as participants. To be included they had to have at least 10 years experience of working clinically with people with CPTSD and they had to be:
- a clinical or deputy clinical lead in a national specialist trauma service; and/or
- holding a senior position in a national or international trauma organisation; and/or
- a leading clinical academic publishing extensively on CPTSD.
Each participant then completed an online semi-structured interview, consisting of 11 open-ended questions, relating to the definition, practical clinical use, composition, key principles, and the evaluation of reintegration. The questions were constructed based on prior literature on CPTSD and with an expert reference group of leading UK trauma clinicians.
Results
Sixteen leading experts were recruited for participation in the study:
- Identified Gender: Female (n=9), Male (n=7)
- Role: Clinical psychologist (n=4), Academic clinical psychologist (n=10), Psychiatrist (n=1), Counselling psychologist (n=1)
- Ethnicity: White (n=13), (White British (n=7), White European (n=1), White Other (n=5)), Mixed Other (n=1), Mixed White (n=1), Asian (n=1)
- Setting*: Public health service (n=10), University (n=10), Private practice (n=3), Charity (n=2)
- Geographical location: England (n=10), Scotland (n=1), Wales (n=1), Switzerland (n=1), United States (n=1), Chile (n=1), South Africa (n=1)
*Several participants worked across more than one setting, e.g. both at university and a public health service.
The interviews were transcribed verbatim and Codebook thematic analysis was used (Braun & Clarke 2019) allowing the researchers to capture areas of consensus along with exceptions and disagreements.
Five main themes were established deductively:
- Definition
- The value of reintegration
- Composition
- Key principles
- Evaluation
Subthemes were then established inductively:
Definition
There was significant variation in this theme, with a shared acknowledgement of the challenge of definition. The main topics discussed included: identity/sense of self, transferring skills from therapy to life, future-oriented thoughts, accessing resources, enhancing life and social strategies.
The value of reintegration
All experts perceived reintegration as an essential part of treatment; adding invaluable transferrable life skills that can be used outside of therapy. Most experts reflected on reintegration specifically being empowering to the person, while giving meaning to the entire course of therapy and neglecting it could result in no change in symptom reduction.
Composition of reintegration
Views about what reintegration should consist of varied significantly across experts however, they all agreed that interventions should be bespoke to the individual. Key examples included: improving functioning, social integration, physical well-being and exercise, occupation, emotion regulation, symbolic rituals, and group work.
Key principles of reintegration
All experts highlighted that a person-centred approach was key and it should be collaborative, and have realistic goals. There was no consensus around who should deliver it, however most experts agreed that the treating clinician should either start or lead the reintegration treatment, but didn’t need to be the sole provider. Most participants believed that reintegration work should start at the very beginning of therapy but with increasing emphasis throughout treatment. Participants struggled to answer how long reintegration should last but a general principle of at least 3 months up to several years.
Evaluation of reintegration
Participants discussed measuring quality of life, wellbeing, global functioning, social adjustment scales, satisfaction, and goal-based outcome measures. With most experts recommending a combination of objective clinical measure and subjective patient-based measures.

The main expert consensus was that reintegration interventions should be person centred and collaborative; evaluated by objective and subjective quality of life measures.
Conclusions
The results of this study start to clarify what the framework of reintegration is/could be and how it can be used. The authors highlighted that consistently discussed themes related to identity, transitioning skills to real life, being future-orientated, accessing resources, and, lastly, enhancing life. There was however far from clear consensus on the definition and composition of reintegration highlighting the need for more specific research on reintegration’s role in the treatment of CPTSD.

All experts perceived reintegration as an essential part of treatment, however, there was significant variation as to the definition and composition.
Strengths and limitations
There is a general lack of literature on this topic, and this would appear to be the first study to explore expert opinion regarding reintegration interventions. The researchers did intentionally include a range of participants from a variety of settings, including different clinical roles, different client groups with CPTSD and a range of geographical locations with the aim of comparing similarities and differences in opinion between clinical settings, which has not previously been examined. The interviews were all held online and by the same researcher limiting any specific variation or bias in the process of the interviews. The use of a standardised coding measure also enhanced the validity of the results.
However, there were only 16 participants making this a very small study and only 4 of these were based outside of the UK. This is a good start in relation to gaining information for reintegration interventions, but much more research is required.

This was small acorn of a study, but from which mighty research oaks may grow.
Implications for practice
In relation to clinical practice there was clear consensus that reintegration interventions are essential when treating CPTSD. I personally, as a psychiatrist, was far more familiar with the stabilisation and trauma memory processing phases of treatment and struggle to recall psychological colleagues discussing the reintegration phase. If this paper can lead to an increased awareness of this invaluable 3rd phase of treatment in clinical practice then this is a good step forward for patients with CPTSD.
There are however much larger implications and opportunities for future research; there still needs to be a consensus on definition, composition, method of delivery and evaluation of reintegration interventions. This feels like an area that is ripe for picking with randomised controlled trials. There may also be a qualitative arm to future research to help understand the nuances of the reintegration phase from a patient perspective.
Concluding, for those patients with CPTSD… you may have to Hold On for a more detailed knowledge base on reintegration interventions.

Increased awareness of reintegration interventions is one of the best outcomes of this paper for patients with Complex PTSD.
Statement of interests
No conflict of interests in relation to this study or publication.
Links
Primary paper
Maria Condon, Michael A. P. Bloomfield, Helen Nicholls & Jo Billings (2023) Expert international trauma clinicians’ views on the definition, composition and delivery of reintegration interventions for complex PTSD, European Journal of Psychotraumatology, 14:1,2165024 https://doi.org/10.1080/20008066.2023.2165024
Other references
Cloitre, M., Courtois, C., Ford, J., Green, B., Alexander, P., Briere, J., Herman, J. L., Lanius, R., Stolbach, B. C., Spinazzola, J., Van der Kolk, B. A., & Van der Hart, O. (2012). The ISTSS expert consensus treatment guidelines for complex PTSD in adults. https://www.istss.org/ISTSS_Main/media/Documents/ISTSS-Expert-Concesnsus-Guidelines-for-Complex-PTSD-Updated-060315.pdf.
Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391. https://doi.org/10.1002/jts.2490050305
Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., Hyland, P., Maercker, A., Ben-Ezra, M., Coventry, P., Mason-Roberts, S., Bradley, A., & Hutton, P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. https://doi.org/10.1017/S0033291719000436