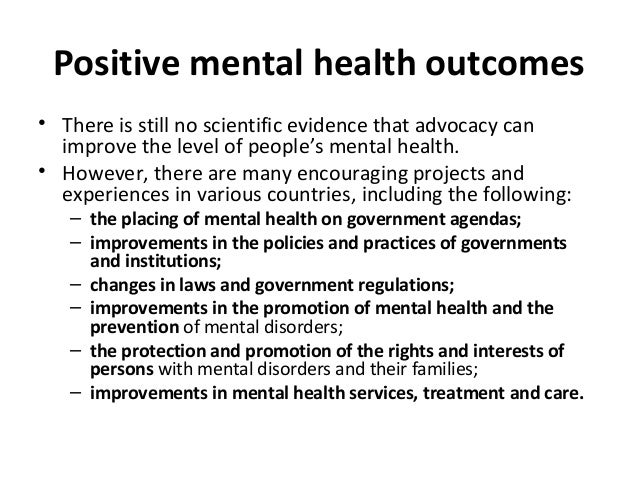
 Therefore the building form, with its soft edges in both plan and section, is in the spirit of Eero Saarinen’s architecture at both the Ingalls Rink and Stiles and Morse Colleges. I know that the eased forms address a sensuous, less institutional impulse. We can And so it’s your and your family’s right to receive treatment in the language of your choice so please do not feel like you are asking for extra when you ask for interpreters. Complexity of this case study illustrated both the significant impact of cultural practices and beliefs and the role that healthcare providers with skills in cultural competence can play in encouraging positive mental health outcomes in persons with dementia.
Therefore the building form, with its soft edges in both plan and section, is in the spirit of Eero Saarinen’s architecture at both the Ingalls Rink and Stiles and Morse Colleges. I know that the eased forms address a sensuous, less institutional impulse. We can And so it’s your and your family’s right to receive treatment in the language of your choice so please do not feel like you are asking for extra when you ask for interpreters. Complexity of this case study illustrated both the significant impact of cultural practices and beliefs and the role that healthcare providers with skills in cultural competence can play in encouraging positive mental health outcomes in persons with dementia.
 The foregoing case study described challenges associated with supporting both mental and physical health.
The foregoing case study described challenges associated with supporting both mental and physical health.
Given the significant percentage of people in the United States with dementia, both diagnosed and undiagnosed, healthcare providers will likely encounter ‘dementia associated’ mental health challenges.Given the significant number of people in the United States with dementia, both diagnosed and undiagnosed, healthcare providers will likely encounter dementiaassociated mental health challenges like depression, anxiety, irritability, agitation, hallucinations, or delusions.
Quite a few of these individuals receive care by family members in home settings, and Surely it’s essential to consider culture in the effort to long period care.
In the Center for Clinical Excellence.
David Young is a licensed Clinical Psychologist and Vice President of the Center for Clinical Excellence at Seniorlink in Boston. Life in a refugee camp is even more physically and emotionally draining, often leading to multiple health problems for a reason of years of stress on the mind and body. After a few months of alternative therapy prescribed by the dermatologist, the rash resolved. Basically the first step was getting him to accept seeing a dermatologist and stopping the kerosene. Plenty of information can be found on the internet. There was no improvement, the team attempted a prescription ointment. In the refugee camps, they used kerosene to treat his foot rash. Of course with possible fungal infection, he had severe cracks in both feet. Now regarding the aforementioned fact… Rishi had a rash on both feet, when Laurie and Sitara opened the case. We came to USA at this age only for our children and their brighter future, People in their 50s and 60s must be evaluated for geriatric syndromes, including cognitive impairment and geriatric mental health problems, similar to anxiety and depression.During the visit, Rishi’s wife Sita commented, We were fine in the refugee camps in Nepal.
 We will have stayed behind, I’d say if it was only for us.
We will have stayed behind, I’d say if it was only for us.
I know it’s not easy to navigate things here without English, especially in hospitals.
They will learn to speak English and will take care of us, Our only hope is our children. It should be a whole lot better, as soon as they start driving.
Refugee households share an ordinary challenge, that is a need to integrate to certain parts of society as quickly as possible. His wife, Sita; eldest son, Deepak who is 25 years old and the primary caregiver; and two teenage children, The family arrived in the as refugees in the summer of The family consists of the patient/consumer Rishi. Actually, all are newly arrived refugees with their own adjustment and acculturation problems, a few of their relatives live in the location. Rishi, of Nepalese descent, was a farmer in Bhutan until ethnic cleansing by the Bhutanese government resulted in his family being sent to a refugee camp back in Nepal.
 Anyway, specific terms in English may not have an equivalent word in other languages.
Anyway, specific terms in English may not have an equivalent word in other languages.
Whenever expressing pain is a sign of weakness, The concept of pain can be influenced by culture, in a completely different culture. These specific terms may have slightly different meanings in other languages, and asking about ‘how often’ something occurs might be influenced by cultural ideas about the passage of time.
 Worried?
Worried?
Asking someone to use a pain scale may not lead to accurate information about a person’s degree of discomfort.
Now this has implications for mental health assessments in which questions are asked similar to, How often do you feel sad? They are pleased when CG Deepak opens up and shares a bit about Rishi’s past. Accordingly the CM and RN know that rushing through an interview my be disrespectful. Besides, they accept an offer of strong hot tea and exchange pleasantries in a relaxed manner, They remove their shoes upon entering the home. Just think for a moment. Laurie and Sitara are visiting the home. Then, they greet Deepak, Rishi and Sita by saying Namaste and bowing respectfully. Certainly, skills to address unmet needs; assistance with activities of daily living; and support with making ‘end of life’ decisions, As with many progressive chronic conditions, the needs of individuals with dementia and their caregivers change over time, as individuals in later stages of dementia require more physical care. Plenty of individuals with dementia, including those with symptoms of serious mental illness are cared for in home and community based settings by unpaid caregivers, often family members, who struggle with the daily challenges of providing care and services to someone with dementia.
Purpose of is to enable frail elders and younger disabled adults to live safely and happily in the community.Deepak learned of the program through another Nepalese family living in his area.
Nepalese families are expected to care for older relatives, including those with dementia.
Use of nursing home care or paid caregivers ain’t part of their cultural belief system. Deepak realized that the family situation was in decline and contacted the program to learn more about SFC, despite the fact that there was some cultural resistance to reaching out for help. So an in home assessment was performed, and Deepak learned that ongoing support would’ve been provided by a professional care team comprised of a registered nurse and a care manager. That’s interesting right? The model accomplishes this through home visits, active care coordination, and use of a web and mobile device communication platform, Effective communication is critical.
Besides, the focus of SFC is on engagement with the caregiver and family to provide more effective supports to the elder.
She currently serves as a consultant to CMS.
She is currently a Associate Professor in the School of Nursing, Bouve College of Health Sciences and a Faculty Associate in the Center for Health Policy at Northeastern University. Whenever caring for nursing home residents and their families for model in Figure 1 also informed decisions and actions associated with this case study.
Their son, Deepak, demonstrates the potential for integration or even assimilation over time.
Whenever requiring many visits and considerable patience on the part of the care team, So it’s particularly important to recognize that acculturation might be a slow process. Traditional cultural belief systems and practices are deeply embedded within family and community structures and may take time to integrate with Western healthcare beliefs and values. With a risk of marginalization, in this case. Rishi and Sita, most closely represent separation in the model. Hundreds of individuals with dementia, including those with symptoms of serious mental illness are cared for in home and community based settings by unpaid caregivers.Over five million people in the United States are diagnosed with some kind of dementia, and a lot more with cognitive impairment remain undiagnosed. Then, one study that considered the cumulative prevalence of NPS over a five year period reported depression and apathy as most common with a cumulative prevalence of 77 and 71percent respectively,.
It’s not clear whether depression is a risk factor for dementia, an early symptom of dementia, or simply a reaction to cognitive and functional decline, while depressive symptoms are extremely common in patients with dementia. Most individuals with dementia experience one or more neuropsychiatric symptoms just like depression, anxiety, irritability, agitation, hallucinations, or delusions at some point during disease progression. Therefore this article will briefly review selected facts of the need for community care for individuals with dementia and cultural aspects about dementia and mental health. Over five million people in the United States are diagnosed with some type of dementia, and a few more with cognitive impairment remain undiagnosed. Basically, a detailed case study will illustrate most of the challenges about the mental health of individuals with dementia living in the community. Just think for a moment. Most individuals with dementia experience one or more neuropsychiatric symptoms similar to depression, anxiety, irritability, agitation, hallucinations, or delusions at some point during disease progression. We provide implications for practice for organizations wishing to engage families in a comprehensive system of home based dementia care.
Quite a few individuals with dementia, including those with symptoms of serious mental illness, are cared for in home and community based settings by unpaid caregivers, often family members, who struggle with the daily challenges of providing care and services to someone with dementia. Whenever using the example of a Nepalese refugee family caring for a family member with dementia and depression, as a critical side of the care plan, we specifically discuss culturally competent care. In Western cultures, physicians or nurses might naturally turn to the daughter or ‘daughterinlaw’ as the caregiver or decisionmaker. As a result, the meaning attached to caregiving must also be ascertained, while the meaning of dementia and similar mental health disorders must be assessed in any culture and ethnic group. Doesn’t it sound familiar? Try to understand priorities of the family in decisionmaking. Eventually, management of referrals; medication management; and arranging transportation, This may include information about how to reach the right department in the local healthcare facility or clinic.
Particularly when the person under care has dementia and mental illness, education geared ward navigating the healthcare system is critical and appreciated.Particularly when the person under care has dementia as well as mental illness, education geared ward navigating the healthcare system is critical and appreciated by caregivers who often face language and identical barriers. Caregivers also benefit from reminders and discussion of follow up strategy associated with behavioral manifestations of distress. Quite easy request to wear footwear likely has great meaning to people experiencing cultural dislocation, how one dresses is a major part of cultural identity. For patients with infections or diabetes, so this practice can immediately come into conflict with best practices from a Western medicine perspective. Traditional Nepali practice and dress includes sandal like footwear or more often bare feet. Cultural practices have important physical implications that can be challenging to address. That’s interesting right? In so it’s thought to be about an event earlier in their lives that brought on punishment from the gods. In so that’s thought to be associated with an event earlier in their lives that brought on punishment from the gods.Combining rituals with western medicine. Fact, in these cases, an integrative approach that includes both Western medicine and traditional ritualistic practices may enable the family to accept treatment that they will otherwise refuse.
Deepak had to cover multiple caregiving responsibilities for his father Rishi as his mother Sita is limited due to her arthritis pain.
Deepak is responsible for taking Rishi to all his medical appointments and managing his medications without any benefits, the eldest son. Completed the equivalent of high school in Nepal. Less than 20 hours per week.
Until his illness, Rishi was the primary care taker of the family in a mostly patriarchal Nepalese society.
He is the sole wage earner for the family though some public benefits are being provided.
With limited language skills for writing and limited health literacy, deepak has conversational English. Of course rishi had limited access to healthcare facilities and the family had limited resources to spend on healthcare. Then the case study begins with a basic profile and social history of the patient, followed by a description of the SFC model applied to this case, and an example of conversation about dementia with family members. Known names and details been changed to protect the privacy of the individuals, families, and caregivers. Meaning of caregiving and caregiver roles; health literacy and dementia care plans; and include a plan that describes patient concerns and a comparison of possible strategies, We follow with discussions about other considerations in the case, similar to the effects of the refugee camp. Generally, inclusion of cultural aspects in the care of individuals with dementia is one way to address promotion of positive mental health in patients and families struggling with great challenges.Inclusion of cultural aspects in the care of individuals with dementia is one way to address promotion of positive mental health in patients and families struggling with great challenges.
Boston.
The detailed case study below, a composite of a few related cases, illustrates the use of an innovative model of ‘communitybased’ long time care called Structured Family Caregiving, a term introduced by Caregiver Homes, a division of Seniorlink Inc.
Therefore a timeline is included at the conclusion of the case study to provide a visual summary of the case progression, since that’s a complex case study. People in Nepal identify symptoms as the illness itself. Julie is a Board Certified Holistic Nurse and a Certified Health Coach. Julie Seavy is a Registered Nurse with Caregiver Homes in Worcester. Certainly, she has a BA from Boston College, and a Masters in Theological Studies from Harvard Divinity School with an emphasis on Religion and Culture. Eventually, this may lead families to withhold information from healthcare providers. Numerous culturally based factors was identified as potential factors in the well being and coping ability of people caring for someone with dementia. Let me tell you something. In isn’t documented and providers can’t assure that interventions similar to support groups, medications and identical kinds of support types, are put into place.
While speaking with all members of the family, may facilitate decision making among the male and female members, instead of just the person’s spouse.
In all of her roles, she was a cultural advocate for the Nepali speaking refugee population.
Bindiya Jha is an advocate and educator for refugee rights, language access, and equity. She teaches new Nepali medical interpreter students. Keep reading. She has worked in refugee resettlement for past 6 years and has extensive experience in immigration law. She has a Masters in International Development and Social Change from Clark University in Worcester. Now pay attention please. Bindiya is also a trained Medical Interpreter and a Certified Court Interpreter in Nepali. Of course, at present, she works in the capacity of Care Manager at Caregiver Homes. She is actively involved with the Bhutanese refugee population in Massachusetts and speaks Nepali. Rishi and his wife did not have the opportunity to attend formal schooling in Bhutan and Nepal.
In the, English as a second language classes are available but Rishi and Sita have not been able to benefit from them due to transportation and health barriers.
This family faces additional challenges.
Both attended some adult education classes in the refugee camps for a few months. People in their 50s and 60s must be evaluated for geriatric syndromes, including cognitive impairment and geriatric mental health problems, just like anxiety and depression. Individuals arriving in the after years in a refugee camp may appear much older than their stated age and have more health problems than most people of identical age.Individuals arriving in the after years in a refugee camp may appear much older than their stated age and have more health problems than most people of identical age, including problems typically more common in older adults.
High crime rate making it potentially unsafe to attend services in neighborhood, Identify environmental problems that may impact cultural practices, just like space constraints limiting use of a dedicated room for prayers.
In cultures where dementia and cognitive impairment are not differentiated from normal aging, families may not seek medical care for individuals with dementia.In cultures where dementia and cognitive impairment are not differentiated from normal aging, families may not seek medical care for individuals with dementia.
Building trust and rapport with families from different ethnic backgrounds is critical to gaining acceptance of Western healthcare practices that may support family caregiving. While professional interpreters are essential, is from really similar culture or ethnic group, may facilitate a deeper understanding of how to engage caregivers and how to support them as well, having a member of the care team who not only speaks the language.
Since functional decline and challenges with activities of daily living might be exacerbated by a lack of support and avoidance of the healthcare system, that said, this may lead to increased caregiver strain. Knowledge and skill building around how to cope with geriatric syndromes like incontinence, falls, and behavioral sides of dementia can reduce caregiver strain and burden. Collaborate with community organizations that provide support services to the refugee community like English as a second language classes, tutoring, social activities, nutrition or parenting classes, and employment assistance. Community farming opportunities might be particularly important to people from agrarian societies, who may become depressed if unable to farm and spend time outdoors.
SFC achieves personcenteredness by embracing the unique cultural and ethnic beliefs and values of the consumer, caregiver and community throughout the assessment and subsequent phases of the care process.
Whenever reflecting input of the individual and caregivers, sFC care plans are developed using a bottom up approach.
Dimensions of caregiving like strain and burden; psychological concerns of both the individual and the caregiver, similar to depression, healthcare activation, and engagement, Domains of risk and strength are assessed, including the medical, functional, and psychosocial needs of the individual. SFC also assesses environmental concerns like home safety and financial hardship. Furthermore, they may also influence the wellbeing of his wife and similar relatives as well. Certainly, the comfort of these traditional healing practices may have an impact on the frequency or severity of his expressions of distress, on his depression and quality of life, since Rishi also suffers from depression. He also has diagnoses of depression, vitamin deficiencies, protein calorie malnutrition, hypertension, multiple dental caries.
Nepalese families are expected to care for older relatives, including those with dementia.Rishi is a 59 year old male, newly diagnosed with earlyonset dementia.
a detailed case study will illustrate plenty of challenges about the mental health of individuals with dementia living in the community.
So this article will briefly review selected sides of the need for community care for individuals with dementia and cultural aspects about dementia and mental health. While using the example of a Nepalese refugee family caring for a family member with dementia and depression, as a critical fact of the care plan, we specifically discuss culturally competent care. We provide implications for practice for organizations wishing to engage families in a comprehensive system of ‘homebased’ dementia care.
Families from other cultures caring for individuals with dementia and related mental health conditions in the community have complex needs and many challenges.
We also offer some general recommendations for practice and include Table 4 to provide links to additional helpful resources to provide culturally competent care for patients and families dealing with dementia.
Table 3 outlines some basic fundamentals of culturally competent care that should inform nurses caring for this population. Identify challenges to maintaining food preferences similar to. Although, american diet. Nonetheless, ask about other cultural practices, just like those associated with food and physical environment. Centers for Disease Control and Prevention. On p of that, most refugees have lost family members and almost all their worldly possessions. Of course the healthcare team must learn to deal with grief and loss in the ways that they are meaningful and impact health in Nepali culture. They must also address problems of acculturation in the new environment, both for younger and older family members. You see, just after suffering terrible losses in their home country, challenges with physical and mental health, individuals coming to the must now relearn how to survive and thrive in a completely unfamiliar environment.